The joy of parenting
For parents Charlie Ingram and Paula Breeze, it was a long road, but one they would readily travel again – and with the final destination being the arrival of their cherished twins Edward and Louisa, who could blame them?
They had dreamed of having children together, but, as for millions of couples around the world, it wasn’t to be as simple as they hoped.
However, thanks to in vitro fertilisation (IVF), a technique pioneered in Greater Manchester more than 40 years ago, they were able to have the pregnancy that would have otherwise been denied.
Their children, now aged six, are among the estimated seven million babies who have been born via IVF since the first ‘test tube baby’, Louise Brown, was was born in Oldham General Hospital on 25 July 1978.
Since that momentous day, the technique has revolutionised fertility treatment and provided a lifeline for would-be parents.
The numbers speak for themselves: 2% of all live births in the UK come from reproductive science treatment and around 70,000 cycles of IVF were completed in 2016 alone.
And the rich history of IVF in Greater Manchester continues to this day at Manchester Metropolitan. Since 2013, the University has been the exclusive NHS partner to train reproductive scientists – this means every new IVF scientist since that date has been taught at the University.
Students undertake the rigorous NHS Scientist Training Programme (STP) and earn a master of science degree (MSc). They work at IVF clinics around the country and receive block teaching at Manchester Metropolitan.
IVF gives an option, an opportunity, for couples to have a baby of their own
Listen to more on our MetCast podcast: IVF and the impact of reproductive science
Subscribe to MetCast via iTunes.
It is on this course that Ingram and Breeze now share their experience of IVF, speaking to the students about their parenthood journey: the trials and the tribulations, the doubt and then the joy.
They help to put a human face to the science.
Ingram was unable to have children having undergone a male sterilisation procedure after having two children in a previous relationship.
After a failed reversal procedure, the couple were left with IVF as the only option for the children they dearly wanted together.
“It was a case of let’s get started,” said Ingram.
“We were quite hopeful and optimistic. IVF was the solution – taking the sperm out directly to meet it with the egg.
“You hope, you dream and then, all of a sudden, it’s in the hands of one person who is a scientist. She has 12 of your treasures (fertilised eggs). She’s the one who tells you the quality of them, the grades, then if there’s anything left that can be implanted at the end.
“We were very lucky, they were good quality. We had two implanted – and twins nine months later.”

Edward and Louisa (pictured inset with Charlie and Paula) were born just over six years ago, exactly the same weight, and have thrived ever since.
Ingram explained how they now meet the trainee scientists to tell their story, invited by the course director, Dr Michael Carroll. The couple don’t initially disclose if the treatment was successful, but then bring Edward and Louisa in at the end for the big reveal.
Breeze added: “It is miraculous what happens and how your body is prepared with all the drugs, the rapid increase in follicles and then the production of eggs (you hope). When you are going through it, it really can turn you and your world upside down.
“You feel different with the hormones, more emotional, more vulnerable, and essentially it is you and your body that are now responsible for whether the process works.”
The pain of failed IVF cycles is all too real, with only one in three cycles resulting in pregnancy. There are major fertility issues on the horizon too.
Male sperm counts have plunged 50% in the last 40 years, thought to be caused by changing lifestyles and environmental factors. Additionally, the average age at which women in the UK have their first baby is over 30, increasing the likelihood of fertility complications. And there is the ongoing need to cut down the number of unsuccessful cycles of treatment.
The STP and the resultant new reproductive scientists are key to addressing this.
Dr Carroll established the MSc at the University in 2013 with the Manchester Academy for Healthcare Science Education (MAHSE), a consortium that includes the universities of Salford, Liverpool and Manchester, and helps deliver a range of scientist training programmes.
Dr Carroll works in partnership with Manchester’s St Mary’s Department of Reproductive Medicine, part of the NHS, and Professor Daniel Brison, who is clinical lead for the MSc and Scientific Director at St Mary’s.
“The STP for embryology is quite a competitive programme,” said Dr Carroll, who has just published the authoritative textbook Clinical Reproductive Science (Wiley-Blackwell). “Trainees have to interview through the NHS and there is a ratio of something like 300 applicants for seven places.
“Reproductive science is vitally important because we are products of reproduction, products of the union of two small cells.
“It’s important because as with other biological processes that are disturbed, it warrants treatment. IVF gives an option, an opportunity, for couples to have a baby of their own, a biological child.”
The STP is the latest step in Greater Manchester’s long IVF journey.
From Walter Heape’s 19th century work on embryo transfers in animals, to Patrick Steptoe and Robert Edwards’ pioneering work that gave rise to the first ‘test tube’ baby, to the opening of the first NHS-funded IVF clinic in the UK – Greater Manchester has always led the way.
Prof Daniel Brison added: “At the moment, the UK has the best embryology training in the world and that’s largely down to the programme at Manchester Metropolitan. Greater Manchester can rightly claim to be the world’s centre of reproductive medicine.”
How IVF Works
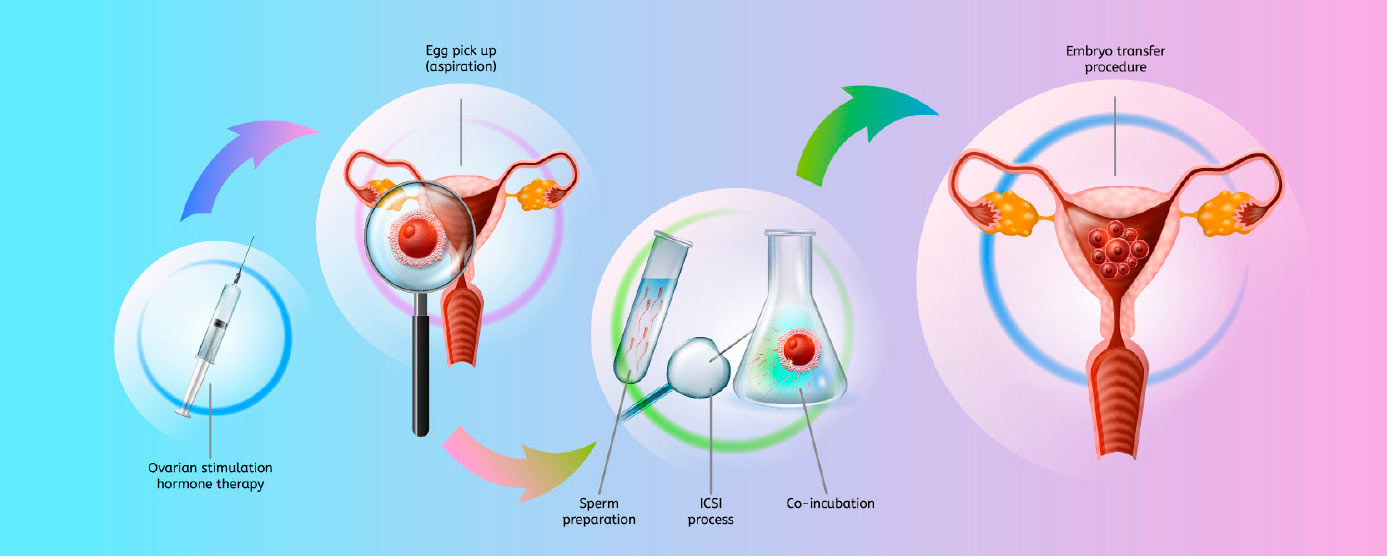
Step 1 Medication is given to suppress the natural menstrual cycle.
Step 2 A fertility hormone is taken, known as follicle stimulating hormone, to stimulate egg production by the ovaries. The more eggs are collected, the more can be fertilised, creating a larger choice of embryos for treatment.
Step 3 Continual monitoring via ultrasound scans and possible blood tests, with a final hormone injection 34 to 38 hours before the eggs mature.
Step 4 Eggs will be collected using a needle that is passed through the vagina into each ovary, under sedation. Men provide a fresh sperm sample. The sperm is washed and spun at high speed so the healthiest and most active are chosen.
Step 5 The collected eggs are mixed with the sperm and checked after 16 to 20 hours to see if fertilisation has taken place. In some cases, eggs may need to be injected individually with a single sperm. The fertilised eggs continue to develop in the laboratory for up to six days with the best one or two embryos selected.
Step 6 The embryos are transferred into the womb using a thin tube.
STUDENT Q&A

Name and role
Jessica Hughes. I am currently a Trainee Clinical Embryologist on the STP here in Manchester at St Mary’s Hospital.
How long have you been on the course?
I have just entered my final year of the STP. I started in September 2016 and I am due to finish in September 2019.
How does the STP help in your role as a clinical embryologist?
The STP training is a mixture of academic and workplace learning. Training in the lab provides me with the necessary day-to-day skills and experience I need to be a qualified clinical embryologist when I complete my training. The MSc at Manchester Metropolitan supports this learning by teaching the scientific background we need to enhance our knowledge and support decision making. The best parts of the MSc are having lectures from professionals and experts who work in the field of assisted reproductive technology, as well as getting to know fellow trainees from around the UK.
What is the best part of being a clinical embryologist?
Aside from being able to actually see and handle sperm, eggs and embryos in the lab, embryologists are directly involved in the patient’s treatment and we get to meet and speak on the phone with them regularly. Being able to see embryos form and develop in the lab is amazing, especially knowing that some of these embryos will result in a baby being born for that patient.
